What is the Australian Multicultural Health Collaborative?
The Collaborative intends to work at the national level to give a voice to the broad health and wellbeing needs, including research, of Australia’s culturally, ethnically and linguistically diverse (CALD) communities.
The Collaborative will represent the voices of wide-ranging CALD health and wellbeing issues at the national level through a formal membership structure which includes CALD consumers, together with health and wellbeing services, health and social care practitioners, researchers, and organisations and institutions for whom the primary focus is health for CALD populations. The Collaborative welcomes as members ‘mainstream’ services and organisations with a significant commitment to CALD health and wellbeing, and will enter into partnerships with relevant national organisations. The title ‘Collaborative’ is significant as an indication as to how members will work – that is, in genuine collaboration on agreed priority areas, drawing on each other’s areas of focus and expertise on particular issues.
There are similar models for a co-ordinated national response from a range of health-related, membership-based and representative groups, including the National Aboriginal Community Controlled Health Organisation (NACCHO), the National Rural Health Alliance (NRHA), the National Ethnic Disability Alliance (NEDA), LGBTIQ+ Health Australia, and the Consumer Health Forum of Australia (CHF). In the multicultural health sector, there are some national organisations with specific interests, including the Refugee Health Network of Australia (RHeaNA) and the Forum of Australian Services for Survivors of Torture and Trauma (FASSTT). They too are membership- based and representative and play significant roles in representing the issues of their constituencies. The Migrant and Refugee Health Partnership (formerly the Migrant and Refugee Women’s Health Partnership), auspiced by Migration Council Australia (MCA), has done significant work, primarily with various medical colleges, in developing clinical competency standards and a guide for clinicians working with interpreters.
The Collaborative acknowledges the important work of RHeaNA, FASSTT, SCoA, RCOA and the Migrant and Refugee Health Partnership and looks forward to supporting and promoting their activities.
Why is the Health Collaborative required?
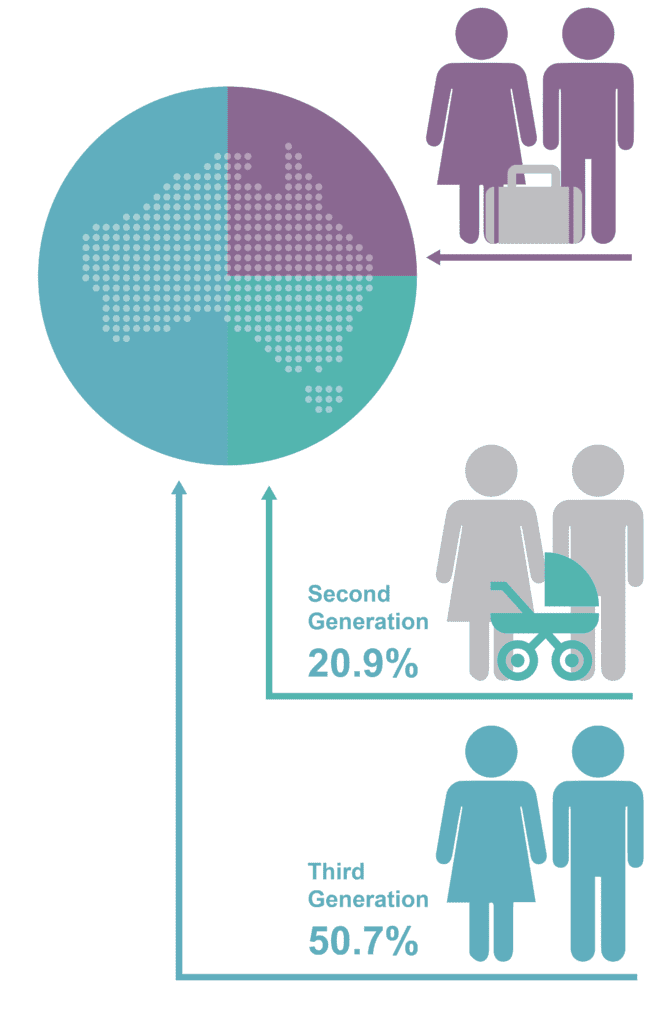
Australians from CALD backgrounds form a significant proportion of the population. The following chart shows an overview of key demographic information derived from the 2016 Census.
The establishment of the Collaborative is all the more timely because the inherent and ingrained health inequities and barriers to access recently exposed by the COVID-19 response have gone substantially unaddressed for decades.
As far back as March 1993, these very same issues were identified and discussed at length in an Australian Government National Health Strategy Issues Paper Removing Cultural and Language Barriers to Health.
The Issues Paper makes many salient observations, including:
In relation to service delivery:
“Community-based services are noteworthy for their relative success in responding to the needs of their local constituencies … assisted with the direct participation of community members from non-English speaking backgrounds in managing their services, and in becoming attuned to local needs and accountability…. Other services have been slow to respond … hospitals and general practitioners do not utilise interpreters to their fullest potential. Services do not cope well with groups with special needs and are frequently not culturally appropriate for ethnic communities.”
In relation to research:
“While there are many small studies, there is no coherent research examining specific health issues for people from non-English speaking backgrounds Data collections are ad hoc and unsystematic. In part this is due to methodological difficulties, but it also reflects the fact that the major health research funding bodies fail to prioritise this issue.”
Nearly 30 years on, the questions must be asked. What has changed for the better? What has not changed, and why not?
This is not to say that no progress has been made. There has been significant investment in migrant and refugee health, both in the community sector and in refugee health and transcultural mental health services within State and Territory Health Departments. In addition, RHeaNA, FASSTT, the Settlement Council of Australia (SCOA), and the Refugee Council of Australia (RCOA) have advanced the health and wellbeing of newly arrived migrants, refugees and asylum seekers. The MCA auspices a Migrant and Refugee Health Partnership. A number of the Primary Health Networks (PHNs) have established dedicated programs/initiatives to address local CALD health issues.
As the COVID-19 pandemic has shown, there are, however, still many issues to be addressed.
It must also be acknowledged that mechanisms are required to ensure that meaningful consideration of the social and cultural determinants of health and prevention are integrated into the development of policy, programs, service delivery and research. At the national level, there must be a stronger focus to address systemic racism and health inequity in our health system to ensure that:
- National health and mental health strategies, plans, initiatives and policy are inclusive of and developed in consultation with and, where possible, co-designed with CALD communities. These should also include targeted strategies for CALD populations and targeted investment.
- Under-representation of these communities in social, health and medical research and clinical trials is addressed.
- National surveys that purport to represent the Australian population as a whole use sampling methodology that explicitly includes Australia’s diverse communities.
- Significant and systemic data deficits in health research and service provision are acknowledged and resolved.
- Engagement with digital health initiatives (such as telehealth, electronic prescriptions and My Health Record) is improved.
- Appropriate language services are available.
- Education, training and support for health practitioners and researchers is enhanced.
- Across the social, and the health and medical research sectors meaningful and genuine consultation, collaboration and co-design occurs.
- The CALD health and wellbeing workforce is appropriately acknowledged and supported.
There is currently no broad national voice for CALD health consumers, for health services working with CALD people, or for health practitioners and researchers who may themselves identify as being from CALD backgrounds.
There are many academics and researchers who have published valuable insights into CALD health issues. However, serious gaps in multicultural health data and knowledge remain without a strategic multicultural health research agenda. Furthermore, all too often CALD people are not well represented in national surveys on health issues and are overlooked or excluded in health and medical research (including clinical trials) where English language proficiency is commonly an inclusion criterion.
Read our Foundation Document
For more information, read the Foundation Document and a one page overview on how the Collaborative works.